Creating the Quiet Zone: Improving noise control in hospitals

By Niklas Moeller
Noise is a well-documented problem in hospitals. In a 2007 study of two facilities, no less than 86 different sources were listed, including patients, staff and visitors talking, and the cacophony produced by televisions, alarms, carts, and doors, along with medical and mechanical equipment.1
In the United States, measures have been taken to encourage hospitals to address this issue, the most powerful of which is the connection the value-based purchasing program has drawn between Medicare funding and Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores. This survey is given to a random sample of patients between 48 hours and six weeks after discharge. The quietness of their rooms was found to be one of the lowest-rated satisfaction markers nationwide, placing noise control at the top of many facilities’ list of objectives.
Though no such legislation currently exists in Canada, noise is a serious issue that nonetheless must be tackled. A growing body of medical studies shows it causes patients more than just irritation. In fact, side effects such as elevated blood pressure, quickened heart rate, and increased metabolism have led researchers to conclude noise even slows recovery rates, lengthening hospital stays.
One of its most serious impacts is sleep deprivation. Sleep is an important part of the healing process, yet noise often prevents patients from getting the rest they need. While it is not responsible for all disruptions, its contribution is significant. Noise reduces both the quantity and quality of sleep, which weakens the immune system and impedes the body’s ability to generate new cells. It can also lead to problems during the day, such as agitation and delirium.2
Further, patients are not the only ones affected. Noise has also been shown to disrupt cognitive and problem-solving capabilities in healthy adults. Though one might think staff can become hardened to noise over time, no one is able to fully tune out these disturbances because senses are designed to detect such environmental changes. Noise disruptions impact caregivers’ concentration, causing stress, fatigue, and errors, potentially affecting quality of care.


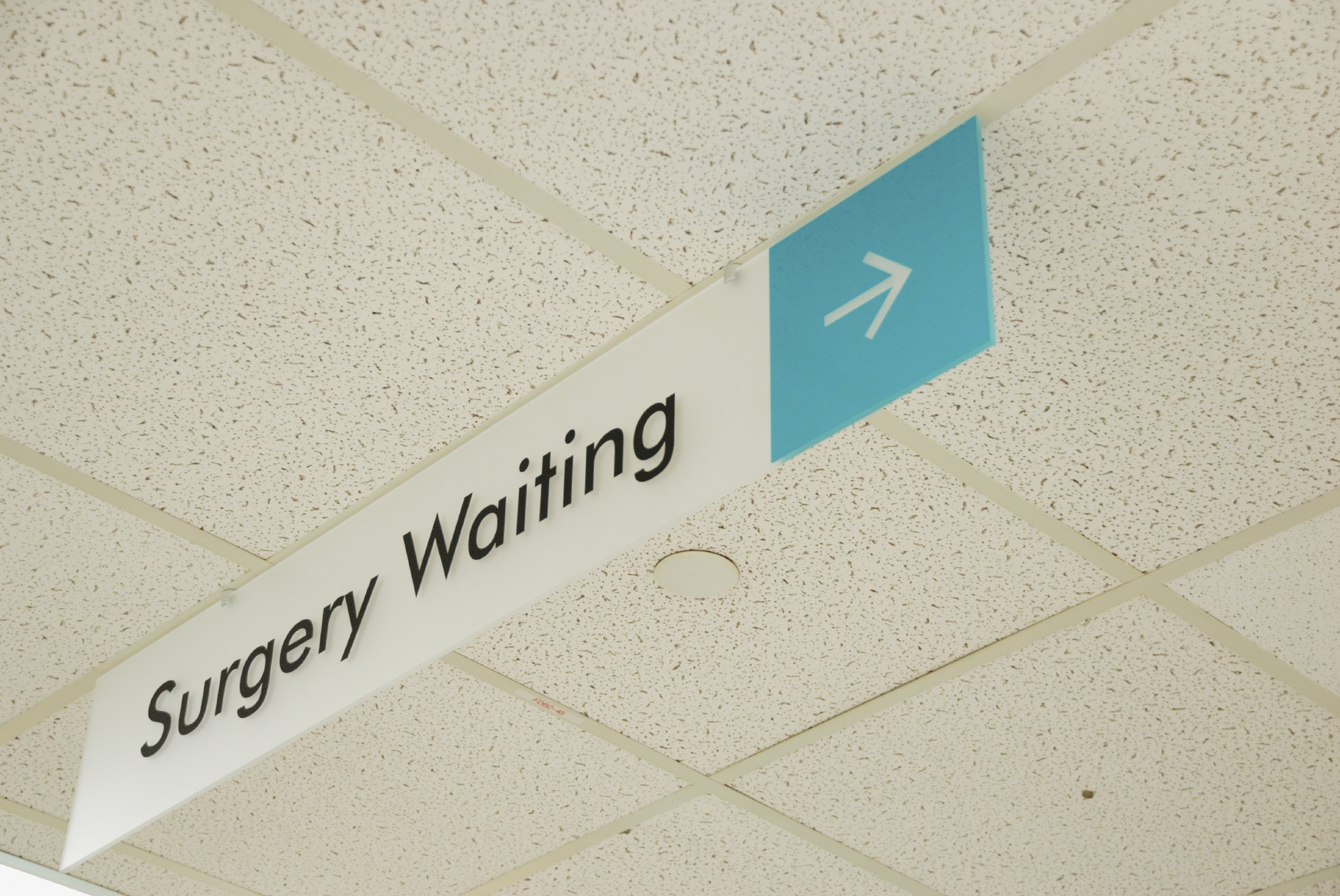
Protecting conversations
Speech privacy is yet another acoustic concern in hospitals. Conversations occur at administrative stations, in hallways and patient rooms. Often, areas used for the input of medical information are located near waiting areas.
South of the border, patients’ right to privacy has been officially recognized in a set of federal regulations developed by the U.S. Department of Health and Human Services (HHS). Introduced in 1996, the Health Insurance Portability and Accountability Act (HIPAA) requires healthcare entities take reasonable safeguards to protect the privacy of verbal communication.
Again, though no such step has been taken in Canada to date, it is difficult to dispute the fact patients have a basic right to a level of auditory privacy. In most situations, having a conversation overheard is merely embarrassing, but in the context of providing healthcare, it is a matter of confidentiality. Further, patients know if they can overhear conversations occurring in adjacent areas, others can hear them as well, making them uncomfortable and less likely to discuss sensitive matters with their caregiver.
The good news is government bodies are taking notice and trying to raise awareness of the importance of auditory privacy.

“I cannot stress strongly enough how important it is to ensure a hospital’s physical assets and infrastructure address the key areas where personal health information is frequently shared,” said Dr. Ann Cavoukian, Information and Privacy Commissioner of Ontario. “Not tackling this issue is akin to keeping sensitive information in a filing cabinet with no locks on it. In both circumstances, the confidentiality and privacy of patients cannot be protected—needless to say, that would be completely unacceptable.”
Reducing noise
If one focuses on the types of noise created by building occupants and small medical equipment rather than structure-borne or mechanical sources, there are four key ways to improve acoustic conditions: reduce, absorb, block, and cover noise.
Each of these strategies contributes differently to the overall result and, therefore, they are best used in combination. When one encounters a problem, its root usually lies in the omission of one or more method or their imbalanced application within the space. Of course, the additional challenge in hospitals is to apply them in such a way so as not to compromise cleanliness or staff’s ability to access patients.
Reducing noise involves identifying, and subsequently reducing or eliminating unnecessary sources of noise within the hospital. Suggestions include:
- lowering the ringer volume on telephones;
- dimming the lights in the evening to encourage quiet;
- fixing or replacing faulty equipment, such as squeaky carts;
- providing training on how to handle loud vocalization by patients;
- purchasing quieter equipment, such as hand towel dispensers and door hardware; and
- limiting or eliminating overhead paging by equipping staff with personal devices.
Changing behaviours can also help reduce noise levels. Some hospitals have formed special committees tasked with raising caregivers’ and visitors’ awareness of noise and enforcing behavioural policies related to its reduction. Anti-noise posters are often topped with clever acronyms, such as ‘SHHH’ (Silent Hospitals Help Healing) and ‘HUSH’ (Help Us Support Healing) or the time-honoured ‘Hospital Quiet Zone.’
Policies for caregivers include:
- promptly responding to alarms;
- changing IV bags before alarms sound;
- restocking supplies during the evening rather than at night;
- talking only in close proximity to the listener, not from a distance;
- using hushed, rather than normal speaking, tones whenever possible;
- asking patients to use headsets and turn off unwatched televisions; and
- designating a ‘quiet time’ during which no routine checks are made unless medically necessary.
Of course, medical device alarms at the patient’s bedside present one of the biggest challenges to noise reduction strategies. A number of more patient- and sleep-friendly solutions have been proposed by manufacturers, such as using wireless technology to direct the alarms only to the relevant doctor or nurse, but concerns remain.
One Johns Hopkins Hospital study showed many existing devices are set up to be ‘overly sensitive,’ resulting in a high percentage of false alarms.3 The research team also found, in many cases, visual indicators would suffice for lower-priority or advisory alarms. Over 10 months, they worked diligently with staff in six units to lower the incidence of alarms. As a result, not only were noise levels decreased, but staff also demonstrated better response due to reduced ‘alarm fatigue.’
Reducing noise in these ways is a great place to start because it means fewer burdens will be placed on acoustic treatments. However, it is impossible to eliminate all noises from a busy, round-the-clock healthcare environment. After best efforts have been made, the remainder of the acoustical burden has to be borne by the design.

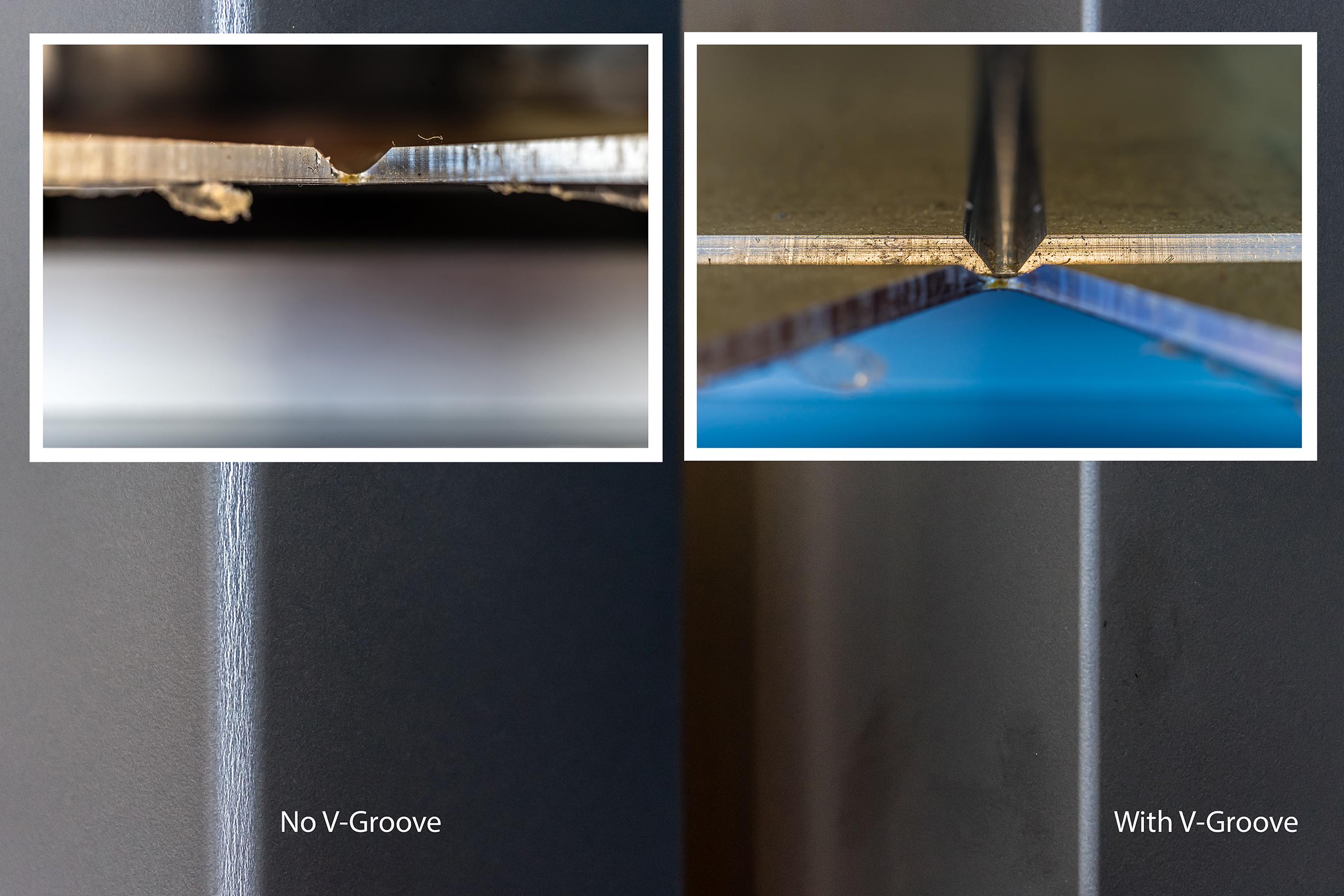
Absorbing noise
Hospitals often feature hard finishes that cause noises to echo, overlap, linger, and travel great distances. Adding absorptive materials that still meet the criteria for sterility and washability will reduce the energy and, therefore, the volume of noises reflected off their surfaces back into the space.
As the ceiling is usually the largest unbroken surface in a facility, a good absorptive tile helps lessen the distance over which noises and conversations can be heard. In fact, a Swedish study determined cardiac patients in rooms with absorptive ceiling tiles were less likely to be readmitted than those in traditional rooms.4
Ceiling absorption is often rated using noise reduction co-efficient (NRC), ranging from zero (no absorption) to 1.00 (100 per cent absorption). Articulation Class (AC) and Ceiling Attenuation Class (CAC) are two additional ratings to consider. The first is the measure of the tile’s ability to absorb noise reflected off the ceiling into neighbouring spaces in open-plan areas in the frequencies important for speech privacy. CAC indicates the tile’s value as a barrier to airborne sound transmission between adjacent closed offices, which is less relevant in hospitals where deck-to-deck construction is typically used. Appropriate tiles should be selected and consistent coverage is ensured throughout the building.
The ceiling’s absorptive power is affected by the type of lighting system used. From an acoustic perspective, the best lighting is an indirect system because it helps maintain the coverage of the acoustical tile across the entire ceiling. It is important to choose a system incorporating a minimum number of fixtures while still meeting the lighting requirements.
Hanging absorptive wall panels may be needed in some situations. They are most effective when applied to large vertical surfaces and key reflective locations, such as corridors. Today, wall panels are available that feature photographs or artwork, not only enhancing acoustics, but also the space’s visual appeal.
Soft flooring can be used to lessen footfall and other ‘traffic’ noise. The challenge for hospitals is to implement it in a manner that does not compromise sanitation or hamper the movement of patients and equipment. Some have purchased motorized beds and use carpet tiles so individual sections can be removed for easier cleaning.

Blocking noise
When it comes to blocking noise, many people immediately think of walls, but a well-planned layout can also be used to minimize direct transmission of sound to and from neighbouring spaces.
For example, high-activity areas and noisy machines such as icemakers should be located in areas well-separated from patient rooms. Doors facing each other across hallways should be offset. It is also helpful to rethink traditional aspects of the hospital landscape. For instance, nursing stations can be decentralized to prevent large groups from talking near patient rooms.
Of course, the most common blocking tactic is to construct closed rooms, but one must keep in mind wall performance is sensitive to gaps—even when deck-to-deck construction is used. Recognizing it is a private room’s biggest Achilles’ heel, some hospitals are re-evaluating their open door policy. However, sound can also transmit through HVAC components, openings under doors, and even back-to-back electrical switches and outlets. Vigilance must be maintained during design, construction, maintenance, and renovation to ensure penetrations are controlled.
In any case, caution needs to be taken when applying blocking strategies, because caregivers need to be able to readily monitor and access patients. When one blocks out noise, the line of sight is also affected.
Covering noise
While most people are familiar with the concepts of reducing, absorbing, and blocking noise, many do not know about the role that sound itself plays in achieving effective acoustics. In fact, these first three strategies are often employed with the objective of making a facility as silent as possible.
There are two fundamental problems with this approach. First, it is impossible to eradicate all noise from a busy, 24-hour healthcare environment. Second, the more silent one tries to make a space, the louder it can seem to occupants. This phenomenon can be attributed to the fact an effective acoustic environment relies in part on the provision of an appropriate noise floor or level of continuous background sound. If it is too low, conversations that are meant to be private can easily be heard and occupants are disturbed by even low-volume noises.
While reducing, absorbing, and blocking perform desired functions—eliminating unnecessary noises, minimizing volume peaks, reducing the distance over which noises travel and the length of time they last—they also lower the background sound level in the space, making remaining noises more noticeable and disruptive. It is also easier for occupants to overhear conversations, even those occurring at a distance or in another room.
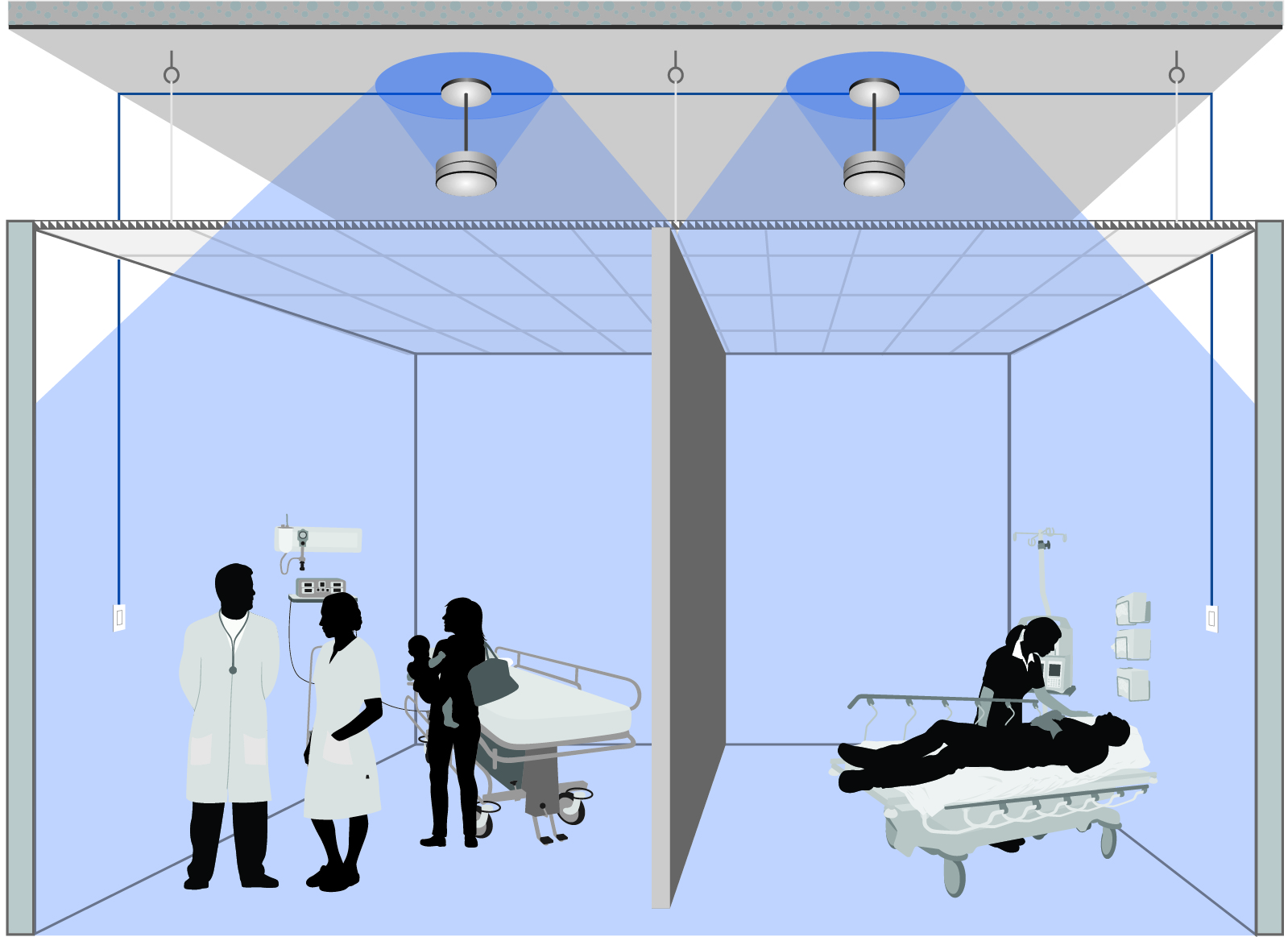
Therefore, though adding more sound to the facility appears to contradict the goal of controlling noise, it is a necessary step—one accomplished by installing a sound masking system. This technology consists of a series of loudspeakers, which are usually installed in a grid-like pattern in or above the ceiling, as well as a method of controlling their output. The loudspeakers distribute an engineered sound most people compare to softly blowing air.
Occupants perceive treated spaces as quieter because this sound covers up noises lower in volume and diminishes the impact of those higher by reducing the magnitude of change between baseline and peak volumes in the space. For this reason, sound masking has also been found to be an effective method of improving sleep. In fact, a 2005 study of intensive care unit (ICU) patients, quality of sleep improved by 42.7 per cent when sound masking was used.5
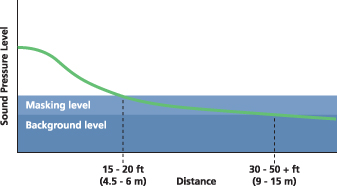
Similarly, sound masking greatly improves speech privacy because conversations are either entirely covered or their intelligibility is reduced. However, masking requires some distance to become effective and, therefore, does not prevent staff and patients from communicating with one another.
Masking also addresses the acoustic variations found within all facilities, which can be due to the type of ceiling, open air return grilles, HVAC equipment, proximity to walls, and machinery. Variations in lighting and temperature are kept within comfortable parameters and, similarly, by introducing a specific background sound at controlled levels across the space, sound masking minimizes variations in both volume and frequency.
To achieve consistency in the often highly fragmented environment of a hospital, the system must be designed to offer small (i.e. one to three loudspeakers) control zones throughout the facility.
Networked control over each small zone is also important in these environments because opening the ceiling has the potential to spread microbiological contaminants, as well as dust, fibres, and odours into the occupied space below. When the system is originally installed in an occupied space, a containment system must be used to provide a seal from the plenum to the floor until the acoustical tile is back in place. One does not want to have to repeat this process when changes need to be made to the sound masking settings or paging/music zones. Therefore, the system should be designed to provide control over all settings and zoning from a location below the ceiling (e.g. via a control panel or software).
The system should also provide patients with the ability to locally adjust the ambient level in their room. In this way, it not only improves comfort, but also increases their sense of control over their environmental conditions, raising satisfaction levels. Central control of individual patient rooms can also be provided at nursing stations. A networked sound masking design can easily integrate with a touch-screen controller and some also offer dedicated PC applications specifically geared to hospital control.
Conclusion
The resolution of noise and speech privacy issues has proven elusive for some hospitals, often due to a misunderstanding of the mechanics of acoustics, which leads to the pursuit of silence. However, just as with other ergonomic factors such as light, temperature, and humidity, the comfort zone for the volume of sound is not zero. Establishing an appropriate background sound level within the hospital not only helps to create a more effective recuperative environment, but it also lets one properly balance the use of absorptive materials and blocking strategies within the space to derive the maximum benefit from the minimum investment.
Notes
1 See D.J. MacKenzie and L. Galbrun’s 2007 article, “Noise Levels and Noise Sources in Acute Care Hospital Wards,” from Building Services Engineering Research and Technology (vol. 28, no. 2). (back to top)
2 This comes from A. Joseph and R. Ulrich’s “Sound Control for Improved Outcomes in Healthcare Settings” (Center for Health Design, 2007) and H. Xie et al’s 2009 piece, “Clinical Review: The Impact of Noise on Patients’ Sleep and Noise Reduction Strategies in Intensive Care,” from Critical Care (13:208). (back to top)
3 For more, see the 2012 report, “Using Data to Drive Alarm Improvement Efforts,” by AAMI Foundation Healthcare Technology Safety Institute (HTSI). (back to top)
4 See D. Bennett’s article in the Boston Globe (May 30, 2010), “Fixing the Noisy Hospital: The Clamor of Modern Medicine can Actually Make Us Worse. So how do you write a prescription for shhh?” (back to top)
5 See M.L. Stanchina et al’s 2005 article, “The Influence of White Noise on Sleep in Subjects Exposed to ICU Noise,” in the sixth volume of Sleep Med. (back to top)
 Niklas Moeller is the vice-president of K.R. Moeller Associates Ltd., manufacturer of the LogiSon Acoustic Network sound masking system. He also writes an acoustics blog at soundmaskingblog.com. Moeller can be reached at nmoeller@logison.com.
Niklas Moeller is the vice-president of K.R. Moeller Associates Ltd., manufacturer of the LogiSon Acoustic Network sound masking system. He also writes an acoustics blog at soundmaskingblog.com. Moeller can be reached at nmoeller@logison.com.